Pancreatic cancer and ways of treating it
Pancreatic cancer, one of the most lethal diseases with a 5-year survival rate over 12% only, claims the lives of over 450,000 people every year. In this essay, we are going to dive into the origins and ways of treating pancreatic cancer.
Throughout history, the origins of pancreatic cancer have always been a mystery. In the late 1980s, the 5-year survival rate for patients with pancreatic cancer was a fraction of 1%, not a lot has been discovered about pancreatic cancer, and doctors regarded the disease as ‘virtually incurable’. Unlike other more common cancers, doctors were unable to find a simple treatment to combat this particular disease, and even palliative treatments were not considered very effective. The most common type of pancreatic cancer (PDAC) was assumed to be from the pancreatic ductal cells, but a study in 2005 proved otherwise. Scientists observed a group of mice with PDAC and found out that it originated from the acinar cells instead. But to this day, there is still a controversial debate to whether PDAC originated from ductal or acinar cells. However, we do know which gene caused the cancer. According to Dr Vogelstein and his teams research in mapping out all the mutated genes in 2008, they found out that 100% of pancreatic cancer contains the KRAS gene mutation, a gene involved in the regulation of cell division.
But what makes this cancer so deadly in comparison to all other cancers? Why does it have such a high mortality rate? Historically, scientists have always thought that the reason behind the lethality is because pancreatic cancer is fast growing and aggressive, but after Dr Vogelstein’s report, we learn that most of the pancreatic cancer has already been in the patients’ body for years. So, by the time doctors realise that their patients have pancreatic cancer, it has probably spread to other areas (such as lymph nodes) or organs, making it too late for any treatments, eliminating hope for recovery. The first symptoms of pancreatic cancer are very non-specific, they include malaise, anorexia, weight loss, change in bowel habit, and epigastric discomfort, then through later development: pruritus, severe back pain and obstructive jaundice. However, if a patient has back pain, it is most likely already too late to resect the tumour. Unfortunately, most patients discover that they have pancreatic cancer at stage IV, which meant that the tumour has already metastasised and spread to other organs, giving them less than 5% chance to live past the next 5 years.
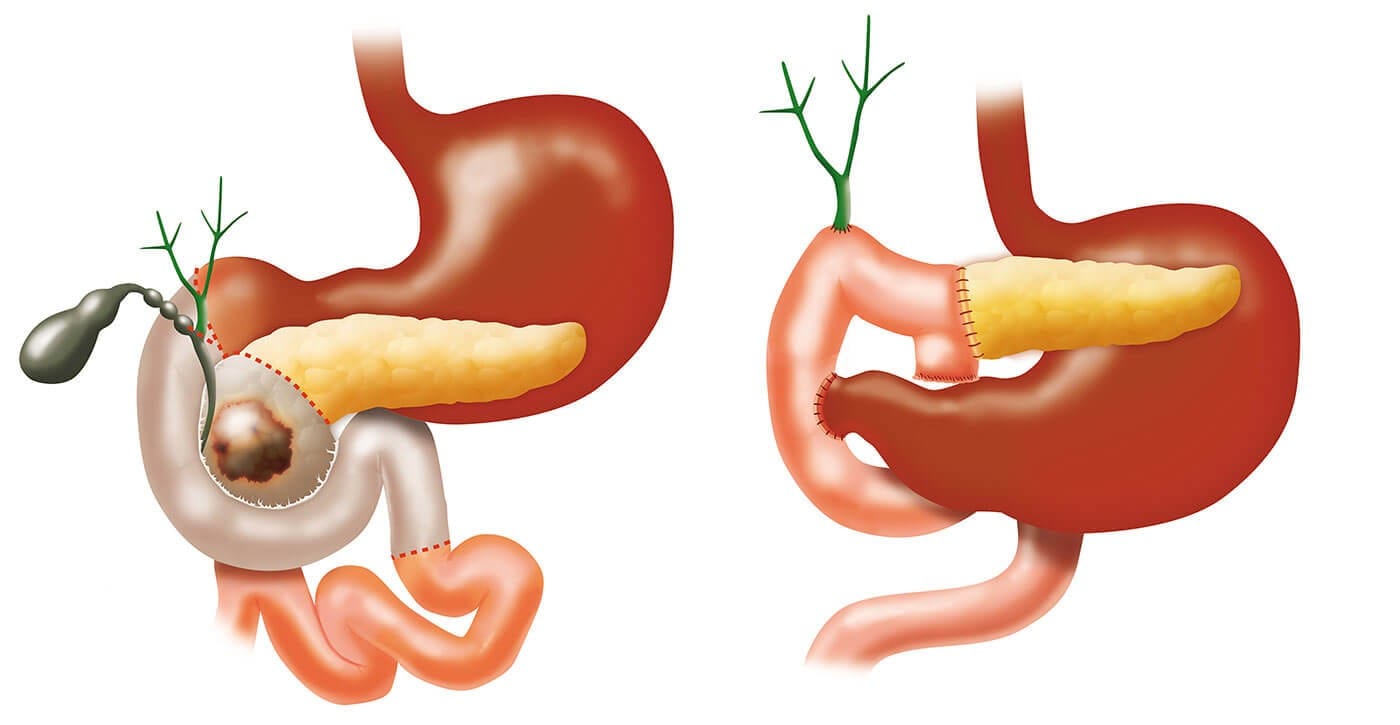
The most common and effective way to get rid of the tumour is surgery, and there are different kinds of surgery to removing it: pylorus preserving pancreaticoduodenectomy (PPPD), Whipple’s operation, distal pancreatectomy, total pancreatectomy and keyhole surgery. These surgeries are recommended to the patients based on the size and stage of their tumours, the location and of course, the patients' health. Whipple’s operation removes the head of the pancreas, most of the duodenum, the gall bladder, and the lymph nodes. Whereas PPPD is a modified version of Whipple’s surgery, which does remove the pylorus and only a part of the duodenum is removed. Both these operations take around 2 weeks for recovery and patients are expected to return to their normal (before cancer) health. Distal pancreatectomy removes the body, the tail of the pancreas and the spleen as well. Keyhole surgery is similar to open distal pancreatectomy; however, it has a longer operation time but a shorter stay in the hospital afterwards. Total pancreatectomy removes the whole pancreas, including part of the stomach, the gallbladder, the bile duct and some lymph nodes. This will take around 6 to 8 weeks for the patient to recover, and the patients must be on antibiotic to prevent infections, then they can start undergoing other treatments such as chemotherapy.
Drugs in chemotherapy work by targeting cells in their different stages of their cell cycles. There are 3 types of drugs in chemotherapy: alkylating agents and platinum-based drugs; antimetabolites; organic drugs.
One of the most conventional and effective method of battling pancreatic cancer is chemotherapy using Folfironox. Approved in 2010, it is a combination of Florouracil (5-FU), Irinotecan and oxaliplatin. Fluorouracil is an antimetabolite, it is converted to flourodeoxyuridylate (also known as f-dump), and that acts as a suicide inhibitor as it forms a covalent complex with an enzyme and it stops the thymidylate synthase, a crucial part in cell division, meaning the cancerous cell could not divide anymore. This is very useful against the tumour cells as they divide a lot quicker than normal cells. Irinotecan is neither of the 3 types of drugs, it is classified as a topoisomerase I inhibitor drug. It works similarly as 5-FU, as it inhibits an enzyme called topoismerase, which prevents cell division completely. Oxaliplatin is an alkylating agent, it is also platinum based (giving the name oxaliPLATIN), the platinum atom forms a covalent bond with the nitrogenous bases, specifically the N7 position of the guanine and adenine, this causes damage to the DNA, resulting in apoptosis.

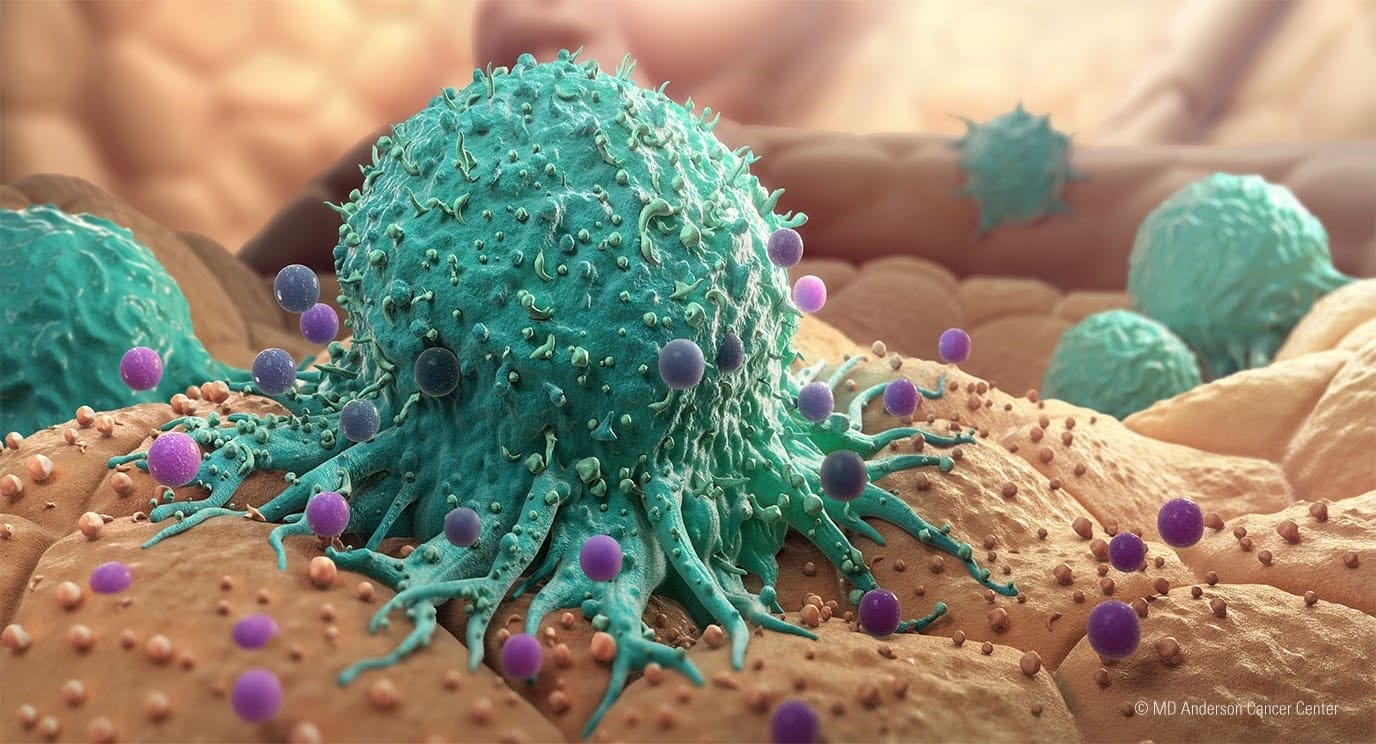
There are 2 types of immunotherapy drugs for pancreatic cancer, Keytruda (Pembrolizumab) and Jemperli (Dostarlimab). They both are immune checkpoint inhibitors, antibodies that binds to a specific receptor on the cell and help the T-cells recognise cancer cells so they could be killed. Immunotherapy is different to chemotherapy as the drugs boosts the t-cells and therefore our immune system to help battle the cancerous cells instead of killing the cancerous cells themselves.
Radiotherapy comes in two types, adjuvant (after surgery) and neoadjuvant (before surgery) radiotherapy. This treatment method is often used as a palliative treatment, aiming to slow the tumour growth, shrink the tumour size and relief symptoms. It works by applying radiation to the cancer cells, damaging the DNA so much that the cancer cells trigger apoptosis. Normally, patients combine radiotherapy with chemotherapy or immunotherapy after surgery to obtain the best results, that is called chemoradiotherapy or radioimmunotherapy. But sometimes, if the patients’ health is not suitable for the side effects of the treatment, they might take radiotherapy as a standalone treatment. However, there are still side effects to radiotherapy itself, if the radiotherapy is quite localised, healthy cells in that specific area might be damaged as a result, causing skin burns or rashes.

There are many other ways of treating pancreatic cancer, but I have covered only the most common ones. To this day, we are still trying to discover better ways of battling the disease, or even just to relieve the symptoms as pancreatic cancer is a painful disease and has such a high mortality rate.
