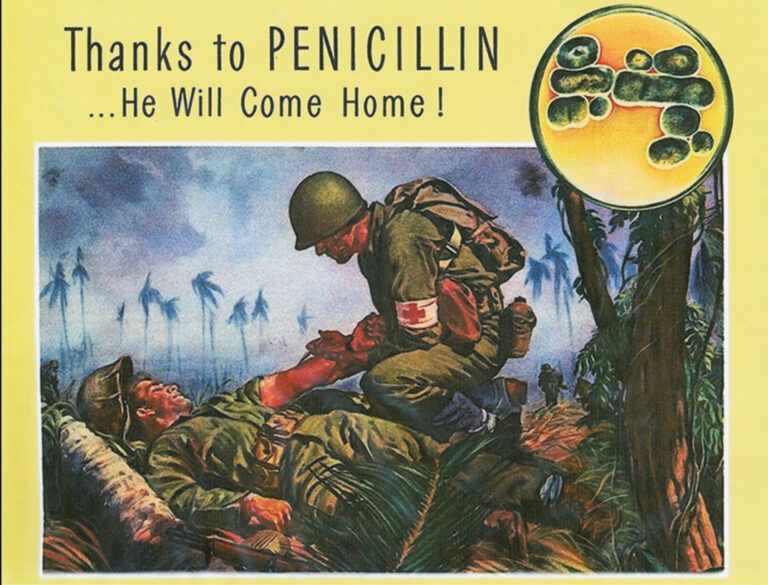
Thanks to Penicillin… He Will Come Home"
When returning home from our travels, the biggest surprise we face is opening our bank balance to reveal the enormous sum of money we have spent, horrified by the expense of our holiday dining. This was not the case for Alexander Fleming. When he returned in September 1928, he was to make one of the most significant discoveries of the 20th century: penicillin, the first antibiotic. A substance now stocked in almost every hospital and surgery worldwide used to fight off the pathogens that cause infection. Little did Fleming know that with the assistance of Florey and Chain, this accidental discovery would change the future of medicine.
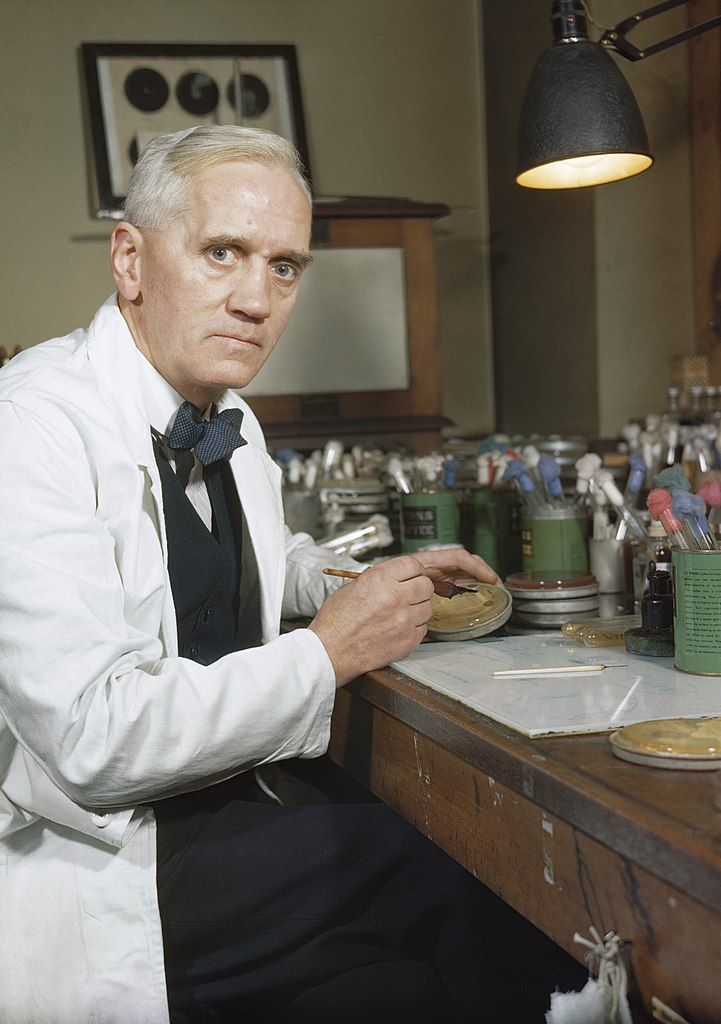
In 1928, Alexander Fleming, Professor of Bacteriology at St. Mary's Hospital in London, investigated the variation of staphylococcal, examining culture plates. Before leaving for a holiday in August, a petri dish of staphylococcus bacteria was carelessly left out on a bench instead of being put in the incubator. The laboratory had several impurities in the air. When he returned, the forgotten petri dish had been contaminated with mould, which caused the dissolution of the bacteria for a considerable distance around it. Understandably, Fleming was more interested in antibiotic substances than staphylococcal variation, and he turned his attention to subculturing the mould and testing it for anti-bacterial properties.
After analysis, Fleming determined that the mould was penicillium fungi. He began testing its antibiotic power on different types of bacteria. He found that some colonies could grow right up to the mould; others, like the staphylococci, stayed a significant distance of an inch away. It was concluded that the penicillium produced an antibiotic substance that could diffuse quickly through agar, only acting upon certain types of bacteria. Many types of bacteria are sensitive to the mould, including pneumococcus, which causes pneumonia and bloodstream infections, and meningococcus, which causes meningitis. It was also discovered that it was non-toxic to leukocytes (white blood cells). This selective antibacterial agent Fleming christened with the inventive name of ‘penicillin’.
In June 1929, Fleming published his findings in the British Journal of Experimental Pathology, suggesting that it could act as a ‘therapeutic agent’ if injected or applied to an area infected with penicillin-sensitive microbes. However, crude penicillin could not be used in medicine just yet. After two weeks, it became inert and destroyed. Concentrating and purifying penicillin would mean this problem could be overcome. However, Fleming’s team of bacteriologists, not chemists, were unsuccessful.
Howard Florey and Ernst Chain and their team at Oxford took up an interest in penicillin in 1938 when conducting a systematic investigation of anti-bacterial substances produced by microorganisms. Even though they found extracting the active ingredient from the mould challenging, as the delicate mould would dissolve in the extraction process, their experiments on mice were highly successful. Penicillin would protect them from staphylococcus, streptococci or vibrion bacteria acting as pathogens. They managed to purify the penicillin using a fermentation vessel, and the Oxford University laboratory became a ‘mini-factory’ producing concentrated penicillin.
At the beginning of 1941, when America was not currently involved in WW2, Florey, alongside biochemist colleague Norman Heatley, travelled to America to stimulate penicillin production in the USA. Pharmaceutical industries became interested and started investing in penicillin extraction, concentration and production. Nevertheless, in December of that same year, when Japanese planes targeted Pearl Harbour, America entered WW2. Penicillin, therefore, did not become simply an antibiotic of scientific interest; it became a necessity. In WW1, half of the ten million soldiers killed were not due to bombs and bullets but to infections or wounds. Allied soldiers fighting on the battlefield of WW2 would still die of infection, such as gas gangrene, even if they recovered from the initial injury.
As part of the war effort, pharmaceutical companies in Britain and the USA (usually competitors) began to collaborate to produce the drug on a mass scale, supported by the government. They worked together to overcome their problems, resulting in most firms producing penicillin by deep-tank fermentation. In 1941, a 43-year-old policeman, Albert Alexander, became the first recipient of the Oxford penicillin. He died shortly after the drug ran out, but its effectiveness was proved. By 1943, the War Production Board (WPB) took on responsibility for increased drug production as it was obvious that this would be incredibly beneficial to the war effort. Twenty-one companies were selected to be part of the penicillin program. They received top priority on construction materials and supplies to meet the high production goals: a primary target was having enough supplies for the D-Day casualties in 1944.
In 1943, there were limited supplies of penicillin. Therefore Dr Keefer of Boston, Chairman of the National Research Council's Committee on Chemotherapy, was assigned the impossible task of rationing the supplies and deciding which patients took priority. The drug was restricted for civilian use and used as a last resort for treatment. However, by 1944, drug companies had increased their output significantly, and penicillin could be used on all infected wounds. The D-Day aim was thus achieved; there was sufficient penicillin to treat all severely wounded Allied soldiers.
Whilst Florey was in the USA, Chain and biochemist Edward Abraham analysed the structure of penicillin in Oxford laboratories. Using X-ray crystallographic technology, they established its molecular structure in 1945. It is a four-membered, highly labile betalactam ring fused to a thiazolidine ring. After further analysis, how the drug functions has also been discovered. Bacteria have a cell wall made of peptidoglycan, which is made by several cross-linkages of peptidoglycan chains synthesised by the enzyme DD-transpeptidase. Penicillin inhibits the action of this specific enzyme, meaning that the cell wall is weakened significantly. Osmolysis then occurs, killing the bacterial cell as it bursts.
Gaynes, R.(2017).The Discovery of Penicillin—New Insights After More Than 75 Years of Clinical Use.
Without Fleming’s accidental discovery, alongside the collaboration and communication between pharmaceutical companies, government, chemists, and biologists, the first antibiotic, penicillin, would not have been made.
The soldiers fighting towards the end of WW2 would not have recovered from their infections, and it is argued that without the discovery, we would not have reached the antibiotic age of medicine. This would mean that we would be much more likely to succumb to infection, with treatments such as organ transplants being hazardous. Today, antibiotics are vital to treating patients, from treating infections to being a safety blanket after an operation has been carried out. The number of lives the drug has saved is immense, and “thanks to penicillin…he will come home”.